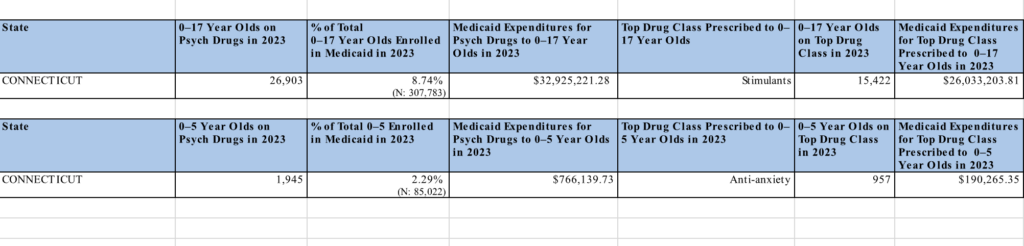
Connecticut Smashes Spending Cap as $5.8 Million Fuels Drugging of Babies Under Medicaid
BREAKING:
Connecticut has shattered its own constitution by breaching the spending cap for the first time in nearly two decades—an unprecedented move that raises alarms about government accountability. The Democratic majority forced through the cap override, while Republican Chairman Ben Proto’s failure to field candidates for many open seats has left the state facing a crisis of taxation without representation.
Beneath this fiscal crisis lies a disturbing reality, Connecticut’s Medicaid program spends $5.8 million a year on psychiatric drugs for children—including hundreds of babies and toddlers. Nearly 400 kids under age four, and even some infants, are prescribed powerful medications like Prozac, often with little oversight. Even the industry, fraught with human rights abuses and coercive practices, cannot justify these actions. As Dr. Andres Martin, a child psychiatrist at Yale, put it: “I can’t make any sense of why a 1-year-old would be on Prozac.” Foster children are especially at risk, being four times more likely to be medicated.